Triple Negative Breast Cancer
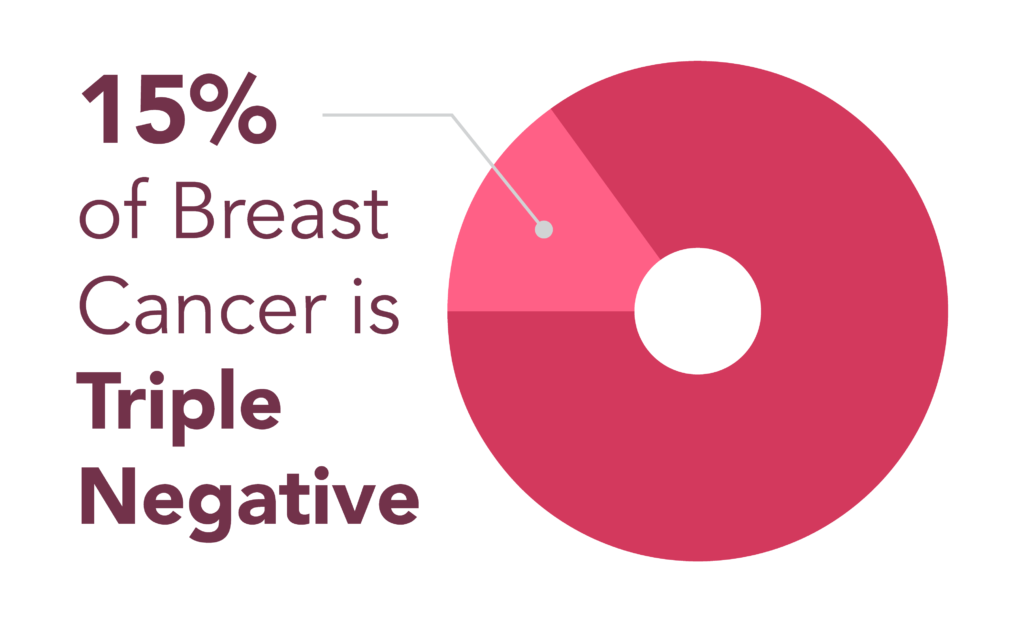
Triple-negative breast cancer (TNBC) is a rare yet fast-growing and aggressive cancer that accounts for approximately 10-15% of all breast cancer cases. TNBC is usually invasive ductal carcinoma (IDC) and has its own specific pathology findings. Because of its tendency to grow and spread quickly, it is important to understand what TNBC is, its signs and symptoms, and the options available to treat it.
Jump to
What is triple-negative breast cancer (TNBC)?
Triple-negative breast cancer statistics and prevalence
What causes triple-negative breast cancer?
Risk factors for triple-negative breast cancer
Triple-negative breast cancer symptoms
Diagnosing triple-negative breast cancer
Triple-negative breast cancer stages
Prognostic factors of TNBC
Triple-negative breast cancer treatment
Prognosis for triple-negative breast cancer
Triple-negative breast cancer research and clinical trials
Triple-negative breast cancer FAQs
TNBC stories of hope
What is triple-negative breast cancer?
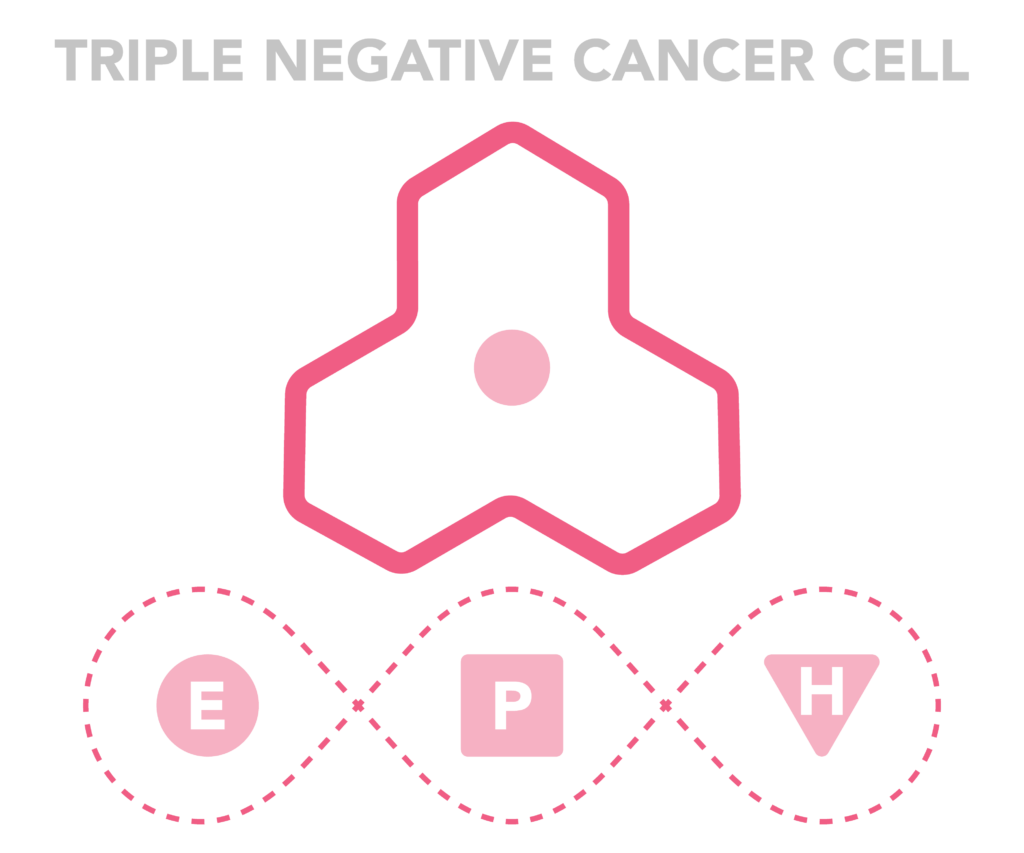
Triple-negative breast cancer is different from other types of breast cancer because it does not contain any of the receptors that are usually found in breast cancer. In triple-negative breast cancer, the three most common receptors known to fuel breast cancer growth—estrogen (ER), progesterone (PR), and the HER2 receptor—are not present in the cancerous tumor. This means that the breast cancer cells have tested negative for estrogen receptors (ER-), progesterone receptors (PR-), and hormone epidermal growth factor receptor 2 (HER2-).
Since TNBC tumor cells lack the receptors usually found in breast cancer (ER, PR, and HER2), common breast cancer treatments like hormonal therapy and drugs that target estrogen, progesterone, and HER2 are ineffective. However, other treatments, such as chemotherapy, can be effective in treating triple-negative breast cancer.
While a diagnosis can be overwhelming, it’s important to remember that early detection and comprehensive treatment can lead to successful outcomes of triple-negative breast cancer.
Triple-negative breast cancer statistics and prevalence
- Triple-negative breast cancer is rare, accounting for approximately 10-15% of all breast cancer diagnoses in the United States.
- TNBC is more common in women under 40 years old than other types of breast cancer. The average age of a TNBC diagnosis is 54, compared to 60 for other breast cancers.
- Black women are nearly twice as likely to be diagnosed with TNBC than white women.
- Those with a BRCA1 gene mutation are more likely to develop triple-negative breast cancer than other types of breast cancer. About 10-15% of women with TNBC test positive for a BRCA1 gene mutation.
Learn more about breast cancer facts and statistics.
What causes triple-negative breast cancer?
While researchers don’t know the exact cause of triple-negative breast cancer, many cases may be linked to a mutation in a breast cancer gene, known as BRCA genes mutations. BRCA is an abbreviation for “BReast CAncer gene.” When a BRCA gene is damaged or changed, it can lead to the uncontrolled growth of tumors, including breast cancer tumors.
While BRCA gene mutations are rare—only 0.25% of the population carries a BRCA gene mutation—about 10-15% of women with TNBC test positive for a BRCA1 mutation, indicating that this mutation may be linked to TNBC in some cases.
Risk factors for triple-negative breast cancer
Traditional risk factors for all types of breast cancer, including lifestyle and environmental factors, also apply to triple-negative breast cancer. However, in addition to traditional risk factors, the following genetic risk factors have been linked to TNBC specifically:
- Age: Premenopausal women and women under the age of 50 have an increased risk of developing TNBC.
- Ethnicity: Black women have higher rates of TNBC than white women, with twice as many Black women diagnosed with TNBC than white women.
- BRCA1 gene mutation: About 10-15% of TNBC in white women test positive for a BRCA1 gene mutation. For Black women with TNBC, about 35% test positive for a BRCA1 mutation.
- Other gene mutations: A mutation in the BRCA2 gene and other gene mutations are also risk factors for TNBC, though to a lesser extent than a BRCA1 mutation.
- Family history: A strong family history of breast cancer of any type and having any type of prognostic factors increases the risk of developing TNBC and other breast cancers.
- Personal history: A personal history of breast cancer of any kind increases the risk of TNBC.
Triple-negative breast cancer symptoms
The symptoms of triple-negative breast cancer are similar to the signs and symptoms of other types of breast cancer. Common signs and symptoms of triple-negative breast cancer may include:
- A new lump or thickening in or near the breast or in the underarm area
- Any unexplained change in the size or shape of the breast, including swelling or shrinkage (especially if on one side only)
- Dimpling anywhere on the breast
- Puckering in the skin of the breast
- A nipple turned inward (inverted) into the breast
- Discharge (fluid) from the nipple (particularly clear or bloody discharge)
- A change in the skin texture, discoloration, swelling, or an enlargement of pores in the skin of the breast (some describe this as similar to an orange peel’s texture)
- Scaly, red, or swollen skin on the breast, nipple, or areola
- Recent asymmetry (unequal or lack of sameness) of the breasts
All changes in your breasts, particularly the ones listed above, should be reported to your healthcare provider immediately.
Diagnosing triple-negative breast cancer
TNBC can be diagnosed through a number of clinical tests, including:
- Diagnostic mammogram: A diagnostic mammogram is performed after a screening mammogram comes back with an abnormal result or if signs and symptoms of breast cancer are present. A diagnostic mammogram provides more in-depth imaging than a screening mammogram.
- Breast biopsy: A breast biopsy is when a tissue sample is taken from a portion of the breast and is examined for the presence of cancerous cells under a microscope in a lab.
- Other imaging tests: Imaging tests such as a breast ultrasound or MRI can also help detect triple-negative breast cancer.
Triple-negative breast cancer stages
Triple-negative breast cancer is staged like other types of breast cancer. Using the TNM scale, breast cancer is assigned a stage based on the size and location of the tumor, whether there is lymph node involvement, and whether the cancer has spread or metastasized. Like other types of breast cancer, triple-negative breast cancer can be assigned a stage of 0 through 4.
Triple-negative breast cancer stages:
| Stage 0 triple-negative breast cancer | Stage 0 TNBC is noninvasive breast cancer that hasn’t spread outside of the milk ducts. It is also known as DCIS. |
| Stage 1 triple-negative breast cancer | In Stage 1 TNBC, the tumor is relatively small, usually less than 2 centimeters. Cancer cells may have spread from the original location into the surrounding breast tissue but have not spread to lymph nodes. |
| Stage 2 triple-negative breast cancer | There are two substages in Stage 2 TNBC: Stage 2A: The cancerous tumor is 2-5 centimeters. Stage 2B: The cancerous tumor is smaller than 2 centimeters but has spread to nearby lymph nodes. |
| Stage 3 triple-negative breast cancer | There are three substages in Stage 3 TNBC: Stage 3A: The cancerous tumor has spread to nearby lymph nodes. Stage 3B: The cancer has invaded the chest wall or skin, such as in inflammatory breast cancer. Stage 3C: The cancer has spread to lymph nodes near the collarbone. |
| Stage 4 triple-negative breast cancer | Stage 4 TNBC means that the cancer has spread to distant areas of the body, such as the bones, liver, lungs, or brain. This is also called triple-negative metastatic breast cancer (mTNBC). |
Prognostic factors of triple-negative breast cancer
Prognostic factors are the characteristics of specific cancers and help determine how cancers are treated. Triple-negative breast cancer cells are characterized by the absence of estrogen receptors (ER), progesterone receptors (PR), and human epidermal growth factor receptor 2 (HER2), making the cancer ER-, PR-, and HER2-.
There are 3 specific prognostic factors that help determine treatment options for TNBC:
- Estrogen receptor status: TNBC is estrogen receptor-negative (ER-) because no estrogen receptors are found in the cancerous cells. This means that the cancerous cells are not stimulated by estrogen to grow and multiply. When the cells are ER-, hormonal therapy will not be recommended as a part of the treatment.
- Progesterone receptor status: TNBC is also progesterone receptor-negative (PR-), meaning that the cancerous cells do not need the hormone progesterone to grow and multiply, which also makes hormonal therapy an ineffective treatment for TNBC.
- HER2 receptor status: HER2, or human epidermal growth factor receptor 2, helps determine how aggressive the cancerous cells are. TNBC is HER2-negative (HER2-) and therefore cannot be treated with drugs that target the HER2 protein.
Triple-negative breast cancer treatment
Because triple-negative breast cancer lacks the receptors commonly found in other types of breast cancer (ER, PR, HER2), treating it with hormonal therapy or drugs that target HER2 is ineffective and therefore not used. However, other treatments are available for triple-negative breast cancer.
Surgery
Surgery is often used as a treatment for triple-negative breast cancer. Common surgeries for TNBC include:
- Mastectomy: A mastectomy is the surgical removal of one or both breasts. If the TNBC tumor is large or has spread into the lymph nodes, or if the patient has tested positive for a BRCA gene mutation, a mastectomy is likely to be performed. A mastectomy will also include lymph node removal.
- Lumpectomy: A lumpectomy, including a sentinel node biopsy, is the surgical removal of the least amount of breast tissue needed to extract the cancerous tumor and provide clear margins around it. If the TNBC tumor is small and has not spread into the lymph nodes, a lumpectomy may be recommended. A lumpectomy for TNBC is typically followed by radiation.
Chemotherapy
Chemotherapy is the most common and effective treatment for triple-negative breast cancer. Depending on the size of the cancerous tumor and if it has spread, chemotherapy may be given before breast surgery (neoadjuvant chemotherapy) to first shrink the tumor and/or cancerous lymph nodes. Chemotherapy may also be given after surgery (adjuvant chemotherapy) to help reduce the chances of the cancer coming back.
Radiation
If the triple-negative breast cancer tumor is larger, or if lymph nodes have been affected, radiation may be given after breast surgery in order to destroy any remaining cancer cells. Radiation uses high-energy rays to kill cancer cells.
Emerging therapies
New therapies are being studied and implemented to treat triple-negative breast cancer. Newer therapies to treat TNBC include:
- Biologic targeted therapy: Biologic targeted therapy uses drugs to block the growth of cancer cells in specific ways. Drugs called poly (ADP-ribose) polymerase (PARP) inhibitors are now being used to treat TNBC.
- Immunotherapy: Immunotherapy uses the body’s immune system to fight the cancer. Immunotherapy is not usually a first-line treatment for TNBC but can be used in certain specific cases.
Prognosis for triple-negative breast cancer
The prognosis for triple-negative breast cancer depends on several factors, including the stage at which the cancer is diagnosed and how well the cancer responds to treatment. Because triple-negative breast cancer is an aggressive and fast-growing cancer, it is more likely to be found at a more advanced stage.
Triple-negative breast cancer survival rates
TNBC survival rates are grouped into three stages: localized, regional, and distant. Each stage has its own 5-year relative survival rate.
5-year relative survival rates for triple-negative breast cancer
| SEER* stage | 5-year relative survival rate |
| Localized: There is no sign that cancer has spread outside of the breast. Includes only invasive breast cancer, not DCIS. | 91% |
| Regional: The cancer has spread outside of the breast to nearby structures or lymph nodes. | 66% |
| Distant: The cancer has spread to different parts of the body, such as the bones, lungs, liver, or brain. | 12% |
| All SEER stages combined | 77% |
**Table information provided by the American Cancer Society
Triple-negative breast cancer recurrence risk
If TNBC recurs, or shows up again, it tends to happen quickly. Most studies suggest that about 75% of TNBC recurrence happens within 3 years of diagnosis, and most within 5 years.
Triple-negative breast cancer can recur as a local recurrence, being found in the breast tissue that remained after surgery, or a regional recurrence, being found in the lymph nodes under the arm or near the clavicle. In a local or regional recurrence, the cancer reappears in the same or nearby area as the original tumor. TNBC may also have a distant recurrence, where the breast cancer cells reappear in other areas of the body, such as the bones, liver, lungs, or brain. This type of distant recurrence is called triple-negative metastatic breast cancer (mTNBC).
Risk factors for triple-negative breast cancer recurrence
The following risk factors have been linked to triple-negative breast cancer recurrence:
- An initial diagnosis of TNBC occurred at age 35 or younger
- Large tumors at the time of initial diagnosis
- Lymph node involvement at the time of initial diagnosis
- More advanced stage of initial TNBC diagnosis
- Undergoing a lumpectomy without radiation to treat TNBC
What You Need to Know About Breast Cancer Recurrence
Learn more about breast cancer recurrence in the free eBook, What You Need to Know About Breast Cancer Recurrence, written by Lillie D. Shockney, University Distinguished Professor of Breast Cancer at Johns Hopkins School of Medicine.
Download the free eBookGood news for triple-negative breast cancer prognosis
It is important to remember that every person’s cancer is different and responds differently to treatment. It is equally important to remember that survival rates are based on other people’s experiences and may not accurately reflect your own experience.
The prognosis for triple-negative breast cancer continues to improve as new treatment methods are discovered and as researchers find new ways to implement existing treatments.
Triple-negative breast cancer research and clinical trials
Research is currently being done to create and improve drug therapies that are specific for triple-negative breast cancer. According to the Mayo Clinic, research advancements in new immunotherapies and targeted therapies, like PARP inhibitors, to treat TNBC are promising.
Some triple-negative breast cancer patients may be interested in taking part in clinical trials, which are research studies that involve people. Triple-negative breast cancer clinical trials look at new ways to treat the disease. The National Cancer Institute (NCI) keeps a list of current NCI-approved triple-negative breast cancer clinical trials. Your doctor will be able to help you determine if a clinical trial is right for you.
Triple-negative breast cancer FAQs
What is the survival rate for triple-negative breast cancer at different stages?
TNBC survival rates are calculated by the American Cancer Society, using data collected from the National Cancer Institute’s SEER database. The SEER database groups cancers into three stages: local, regional, and distant.
- Local (typically Stages 0-1): More than 90% of people were alive 5 years after a TNBC diagnosis.
- Regional (typically Stages 2-3): More than 65% of people were alive 5 years after a TNBC diagnosis.
- Distant (Stage 4): More than 10% of people were alive 5 years after a TNBC diagnosis.
How is the aggressiveness of triple-negative breast cancer compared to other types of breast cancer?
Triple-negative breast cancer is considered more aggressive than other types of breast cancer. This is due to several reasons, including:
- The cancerous cells in TNBC grow and spread more quickly.
- The tumor grade of TNBC is usually high, typically Grade 3, meaning that the cancerous breast cells look very different from normal breast cells and are growing quickly.
- There are fewer options for treatment since hormonal therapy is ineffective for TNBC.
- TNBC has a higher risk of recurrence than other types of breast cancer.
How quickly can triple-negative breast cancer progress?
Triple-negative breast cancer tends to progress (grow and spread) more rapidly than other types of breast cancer. Studies have shown that TNBC tumors can grow by 1% each day. By comparison, the daily growth rate of HER2-positive breast cancers is 0.859% each day.
Triple-negative breast cancer stories of hope
Shortly after turning 40, Shannon was diagnosed with triple-negative breast cancer. Read Shannon’s 7 Takeaways From a Triple Negative Breast Cancer Survivor to find hope in the midst of a TNBC diagnosis.
Sources:
American Cancer Society
American Cancer Society
American Cancer Society
National Institutes of Health
Cleveland Clinic
Moffitt Cancer Center
Moffitt Cancer Center
Johns Hopkins Medicine
American Association for Cancer Research
Medical News Today
Medical News Today
Mayo Clinic
National Institutes of Health



