Lab Tests
If you are diagnosed with breast cancer, your doctor will order additional lab tests to assist with prognosis. The two most common lab tests are the hormone receptor test and the HER2/neu test. Results from these tests can provide insight into which cancer treatment options may be most effective for you.
Testing The Tumor Cells For Hormone Receptors
A hormone receptor is a specialized protein located on the surface of or within a cell. The receptor binds to the female hormones estrogen and progesterone, which flow through the blood. Once bound, the hormone signals the cell to start growing and multiplying.
Many breast cancer tumors contain hormone receptors, often in large numbers. When hormone receptors are present, estrogen and/or progesterone can fuel the growth of the cancer. Such hormone-dependent cancers often respond well to hormone therapy, which differs from hormone replacement therapy (HRT). If neither estrogen receptors (ER) nor progesterone receptors (PR) are present, the cancer is said to be “hormone-receptor-negative,” and hormone therapy would likely be ineffective. Knowing whether the cancer cells have hormone receptors can be valuable to your medical team and your treatment plan.
Who Needs Hormone Receptor Testing?
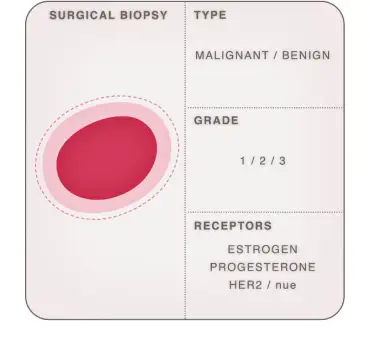
Hormone receptor testing is generally recommended for all breast cancers, including DCIS. If your doctor orders this test, you may be asked to discontinue taking any prescribed hormones for a period of time before the breast tissue sample is obtained. Usually, the sample comes from a biopsy, but the test may also be performed on tissue removed during a lumpectomy or mastectomy. It is standard of care however to obtain these types of pathology results on biopsy tissue.
How Does The Test Work?
The testing lab typically uses a specialized staining process on the breast tissue sample to see if hormone receptors are present. The technical name for this procedure is an “immunohistochemical staining assay” or an “ImmunoHistoChemistry (IHC).” Findings will be included in a pathology report given to your doctor. If the cancer is deemed “estrogen-receptor-positive” (ER+), its cells have receptors for the estrogen hormone. That means that the cancer cells likely receive signals from estrogen to promote growth. About two out of every three breast cancers contain hormone receptors.
If the cancer is progesterone-receptor-positive (PR+), its cells have receptors for progesterone. This hormone could then promote the growth of the cancer.
The cancer cells being estrogen and/or progesterone receptor-positive (hormone positive) is a good prognostic factor to have, usually leading to a better prognosis.
What do the results of hormone testing mean?
Breast cancer patients who test positive for both estrogen receptors and progesterone receptors usually have a better-than-average prognosis for survival and a complete recovery than those who have no receptors present. Also, the more receptors and the more intense their reaction, the better they respond to hormone therapy. Patients with one type of receptor but not the other may still reap benefits from this form of treatment, but likely not to the same degree. As mentioned earlier, if the cancer is both ER- and PR-negative, it probably won’t respond to hormone therapy. Typical response rates to hormone therapy are as follows:
- ER and PR positive: 75-80%
- ER positive and PR negative: 40-50%
- ER negative and PR positive: 25-30%
- ER negative and PR negative: 10% or less
HER2/neu Test
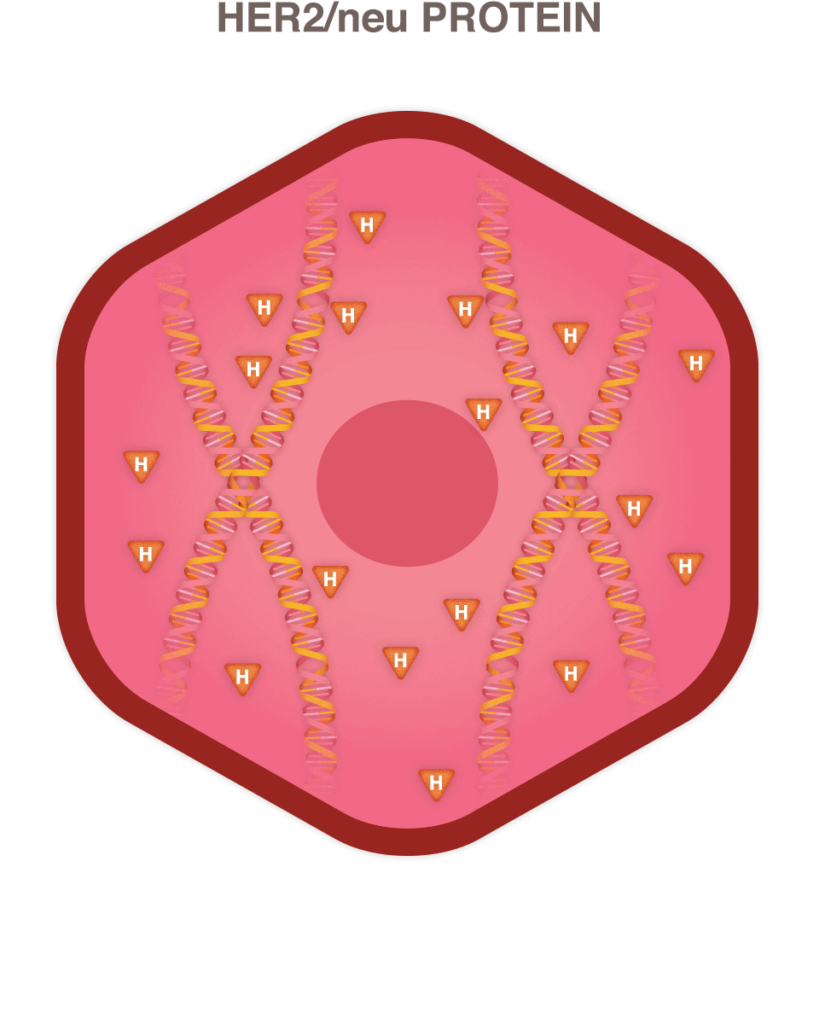
Similar to the hormone receptor test, the HER2/neu test looks for a specific kind of protein that is found with certain types of cancer cells and the gene that produces it. The formal name of that gene is the human epidermal growth factor receptor 2, and it makes HER2 proteins. These proteins are receptors on breast cells.
In a sense, genes contain the formula for the number and combination of proteins a cell needs to remain healthy and function properly. Certain genes and the proteins they create can determine how breast cancer progresses, as well as how it responds to various types of treatment.
What is a HER2 receptor and how does it relate to breast cancer?
Healthy HER2 receptors are the proteins that help manage how a breast cell grows, divides, and repairs itself. However, in about a quarter of all breast cancer patients, the HER2 gene isn’t functioning properly. It makes an excess number of copies of itself in a process known as “HER2 gene amplification.” Then these extra genes instruct the cells to make too many HER2 receptors, which is called “HER2 protein overexpression.” The ultimate result is that breast cells grow and divide in an uncontrolled fashion.
The HER2/neu test can discover whether the sample is normal or whether it has too much of the HER2/neu protein or an excessive number of copies of its gene. If you have been diagnosed with invasive breast cancer or have had recurrent breast cancer, your doctor may recommend this test. It will help your oncology team determine your prognosis, characteristics of the tumor including how aggressive the tumor is likely to be, and the best treatment options.
This test is often ordered in conjunction with the hormone receptor test. Typically, the breast cancer tissue sample from a biopsy or the tumor removed during a mastectomy is used. This test can take about a week to get the pathology results back, whereas determining if the cells are cancer usually is known in just a day or two.
What will the HER2/neu results tell me?
There are four tests for HER2, and results of these may appear on your pathology report, which may take several weeks to come back.
The first one is the IHC test, which is short for “ImmunoHistoChemistry.” It looks at whether there is excess HER2 protein in the cancerous cells. A result of 0 or 1+ indicates there is no excess, 2+ is borderline, and 3+ means the cells test positive for HER2 protein overexpression.
The remaining three tests all examine if the cells contain too many copies of the HER2 gene. These tests include:
- The FISH test (“Fluorescence In Situ Hybridization”)
- The SPoT-Light HER2 CISH test (“Subtraction Probe Technology Chromogenic In Situ Hybridization”)
- The Inform HER2 Dual ISH test (“Inform Dual In Situ Hybridization”)
There are three possible results for these tests: positive (meaning HER2 gene amplification), negative (indicating the number of HER2 genes is not excessive), or low (provides some patients with advanced breast cancer the opportunity to receive therapy that is specific for HER2/neu positive breast cancer patients).
In the pathology report, breast cancers with HER2 protein overexpression and HER2 gene amplification are called HER2-positive. This type of cancer often grows faster, spreads to other areas more readily, and has a higher likelihood of recurring versus HER2-negative breast cancer.
When all three of the tests come back negative for receptors for hormones (progesterone and estrogen) and negative for HER2, triple negative breast cancer may be the diagnosis.
Materials on this page courtesy of:



